While some degree of menstrual discomfort is not unusual, severe pain may be a sign of a problem.
Normally, menstruation comes with some degree of discomfort. However, when menstrual pain is severe, it can be a sign of a problem. Fortunately, most of these causes can be treated. If you are experiencing severe menstrual pain, see your doctor, so he or she can help you figure out what is causing your pain.
What is normal menstrual pain?
Menstruation can be uncomfortable. Your breasts may be tender for a day or two, you may have cramping in your lower abdomen, and your back may ache. This type of pain usually lasts 1-4 days. Heat packs and over-the-counter pain medications, such as ibuprofen or acetaminophen will help with typical menstrual cramps, as will avoiding constipation.
When is menstrual pain not normal?
Your menstrual pain may be a sign of a problem if you have:
- Pain so severe that over-the-counter pain relievers are not helping
- Intense backache
- Pain so severe that you cannot participate in your normal activities
- Severe diarrhea or constipation, or blood in the stool
- Bladder pain
- Pain during intercourse
- Symptoms at times other than your period
If you have severe symptoms as listed above, see your doctor. One of the most common causes of intensely painful menstruation is endometriosis . Endometriosis, and other causes of severe menstrual pain can be treated. For more information on endometriosis, see this section.
What can I do to reduce cramps?
Menstrual cramps can be quite painful, but there are a few things you can do to help get some relief:
Heat
Have a soak in warm bath, or use a hot water bottle or heating pad on your abdomen.

Anti-inflammatory medications
These include ibuprofen and naproxen. These are most effective if you start taking them a day or two before your period is expected to arrive.
Hormonal birth control
The birth control pill or other hormonal methods of birth control (e.g., the patch, vaginal ring, shot, IUD) can be used to significantly reduce your menstrual cramps.
Why do I have problems with my bowels when I have my period?
It is common to find that your bathroom habits change while you are menstruating. The hormones that regulate the menstrual cycle also affect the bowel. For example, your body produces a higher level of prostaglandins when you are menstruating. Prostaglandins are responsible for causing uterine contractions, but can also cause your bowels to contract. Right before your period starts, you also have an increase in progesterone, which can slow down your bowel contractions. Because of these chemical changes in your body, you may experience constipation or diarrhea.
Diarrhea
Many women find that they experience more frequent bowel movements during their periods, and many have episodes of diarrhea in the first day or two of menstruating. Ibuprofen works by blocking prostaglandin production, so if you have a lot of trouble with loose bowels, ibuprofen can help.
Constipation
Due to the slowing of bowel contractions just prior to menstruation, it is common for to experience constipation around the onset of your period. Be sure to drink lots of water, eat plenty of dietary fibre (beans, peas, fruits, vegetables, whole grains), and get some exercise to help alleviate the discomfort of constipation.
Existing bowel problems
If you have ongoing problems with your bowels, such as irritable bowel syndrome (IBS), your bowel symptoms may worsen during your period. You may also have more cramping and other PMS symptoms. Some women with IBS find that using the birth control pill improves the bowel symptoms associated with menstruation.
What are the causes of painful periods?
Endometriosis
For more information on endometriosis, click here .
What is endometriosis?
Endometriosis happens when the type of tissue that normally lines the uterus (called the endometrium), grows in other places within her body, usually somewhere in the abdomen.
What causes endometriosis?
 The cause of endometriosis is not understood, there are several theories. In some women menstrual blood containing endometrial cells travels backwards, up through the fallopian tubes, and into the abdomen. In others, tissue of the type that normally lines the uterus, develops in other parts of the abdomen or pelvis. The tissue appears less responsive to the female hormone progesterone. A genetic factor has also been identified. Whatever the cause, in too many women the diagnosis comes late, after years of suffering. And early diagnosis is important.
The cause of endometriosis is not understood, there are several theories. In some women menstrual blood containing endometrial cells travels backwards, up through the fallopian tubes, and into the abdomen. In others, tissue of the type that normally lines the uterus, develops in other parts of the abdomen or pelvis. The tissue appears less responsive to the female hormone progesterone. A genetic factor has also been identified. Whatever the cause, in too many women the diagnosis comes late, after years of suffering. And early diagnosis is important.
What are the symptoms of endometriosis?
The symptoms of endometriosis include painful menstrual cramps, painful intercourse, diarrhea, constipation, and nausea. The symptoms are different in different women.
How does endometriosis affect a woman’s health?
Endometriosis can cause many problems for a women, apart from painful periods. Endometriosis can cause painful cysts on the ovaries, puckering ad scarring in the tissues that line the pelvis, and can affect other structures in the pelvis and abdomen, such as the fallopian tubes, the bladder the bowel, and the wall between the vagina and the rectum. In some cases endometriosis can impair fertility
How is endometriosis diagnosed?
Your doctor will want to know about your menstrual history, your pain and other symptoms, medical history, family history of endometriosis, and your general health. You may also have a pelvic exam, rectal-vaginal exam, and an ultrasound. If you have widespread endometriosis you may also require other imaging tests such as colonoscopy , cystoscopy, rectal ultrasound, or MRI .
How is endometriosis treated?
The first step in living with endometriosis is being sure you are leading a healthy lifestyle.
Endometriosis is often accompanied by bowel problems, such as irritable bowel syndrome, bladder pain such as interstitial cystitis, and pain arising from the pelvic floor muscles. Addressing these main contributors to pain will greatly help with endometriosis symptoms.
Menstrual pain from endometriosis may be managed with ibuprofen or naproxen. Progestins can also be helpful in controlling endometriosis, so hormonal birth control methods (the pill, patch, vaginal ring, IUD, or shot) that contain either estrogen and progestin, or progestin alone, will help many women.
Continuous hormonal contraception may be prescribed, where menstruation is suppressed by not taking the usual 7-day break from the birth control pill. Other medications that suppress menstruation may be effective, such as progestins that are more effective against endometriosis (Dienogest) a progestin IUD, GnRH agonists (gonadotropin releasing hormone) or danazol. In some cases of endometriosis where pain is severe and not responding, fertility is compromised, or a mass found, surgery will be advised.
Fibroids
For more information on fibroids, click here .
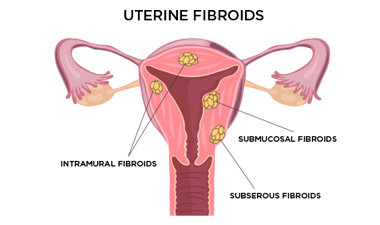 What are fibroids?
What are fibroids?
A uterine fibroid is a non-cancerous tumour that grows from the muscle cells in the uterus. It has the appearance of a whorl of muscle fibres. Fibroids range in size from a few millimetres to 10 cm or more.
What causes fibroids?
The exact cause of fibroids is unknown, but hormones and growth factors seem to play a role.
What are the symptoms of fibroids?
Fibroids may grow without causing any symptoms, but may cause heavy menstrual bleeding, a sensation of pressure or pain in the pelvis, frequent urination, constipation, leg pains, or backaches.
How are fibroids diagnosed?
Based on your menstrual history and the symptoms you have, your doctor may suspect fibroids. He or she may also be able to feel fibroids during a pelvic exam. To diagnose fibroids ultrasound (either abdominal or transvaginal), and blood tests to rule out other disorders are required. Sometimes other imaging tests such as MRI, hysterosonography, or hysteroscopy may be recommended
How are fibroids treated?
The treatment for fibroids depends on the size and number of fibroids, the symptoms they are causing, and the preference of the woman. Hormone treatments can shrink fibroids. Non-hormonal medications, such as tranexamic acid can be taken during menstruation to reduce heavy bleeding. There are also procedures that can destroy or remove uterine fibroids.
Uterine infections
What is a uterine infection?
An infection of the female reproductive organs can be caused by a number of different bacteria, including chlamydia, gonorrhea, ureaplasma, mycoplasma, and others. These infectious agents cause a condition known as pelvic inflammatory disease (PID).
What causes a uterine infection?
Sometimes PID is caused by a sexually transmitted infection , such as gonorrhea or chlamydia. Other risk factors include the use of an IUD, and douching.
What are the symptoms of a uterine infection?
Some infections (like chlamydia) can have no symptoms at all. Symptoms of a uterine infection may include pelvic pain, heavy menstrual bleeding, foul smelling discharge, bleeding between periods, pain during sex or urination, and fever or chills.
How is a uterine infection diagnosed?
Your doctor may suspect you have a uterine infection based on your symptoms. The diagnosis can be confirmed with a pelvic exam, taking a swab of your cervix, and testing your urine. You may have other tests to see if any of your pelvic organs have been damaged by the infection, such as a pelvic or transvaginal ultrasound or an endometrial biopsy.
How is a uterine infection treated?
Usually a uterine infection is treated with antibiotics. If the cause of your uterine infection was a sexually transmitted infection, your partner should also be treated.
Pelvic congestion syndrome
What is pelvic congestion syndrome?
Pelvic congestion syndrome is a condition where an accumulation of dilated, convoluted veins (like varicose veins) occurs in the pelvic area, causing pain that can be quite severe. It is also associated with heavy menstrual bleeding.
What causes pelvic congestion syndrome?
Pelvic congestion syndrome is caused by a failure of the valves in the pelvic veins surrounding the ovaries. This causes the blood in the veins to pool, and the vessels to become engorged and painful. Why the valves in the veins fail is not known. Women who have had more than one baby are more likely to develop pelvic congestion syndrome.
What are the symptoms of pelvic congestion syndrome?
The primary symptom of pelvic congestion syndrome is pain. Pain in the lower torso that is worse after intercourse, during menstruation, or after activities such as horseback riding, may be caused by pelvic congestion syndrome. Heavy periods are also associated with pelvic congestion syndrome.
How is pelvic congestion syndrome diagnosed?
Dilated veins can be difficult to see with the typical tests used to feel or visualize the pelvic organs, such as a pelvic exam, ultrasound, or hysteroscopy. A diagnosis of pelvic congestion syndrome is usually one that arises when other conditions have been ruled out. MRI is the best test for viewing dilated veins.
How is pelvic congestion syndrome treated?
Treatment of pelvic congestion syndrome can include hormone medications that reduce the flow of blood to the veins. Another treatment is called embolization. This is where a doctor inserts a thin tube called a catheter into a vein in your leg, and guide it to the vein that is causing problems. The vein will then be blocked with a small coil, sponge, or glue, so that blood can no longer pool in the treated veins. This treatment has a high success rate.
Ectopic pregnancy
What is an ectopic pregnancy?
An ectopic pregnancy happens when a fertilized egg implants into the fallopian tube or elsewhere in your body. An ectopic pregnancy is not viable, and requires emergency treatment. This is because the pregnancy can cause the fallopian tube to rupture and can cause severe bleeding.
What causes an ectopic pregnancy?
It is not clear why ectopic pregnancies happen. In some cases, damage to a fallopian tube can prevent the fertilized egg from being able to descend into the uterus. Increased risk of having an ectopic pregnancy is associated with pelvic inflammatory disease, sexually transmitted diseases, and fertility treatments.
What are the symptoms of an ectopic pregnancy?
You may have no symptoms at all and the pregnancy may be diagnosed by ultrasound, or it may rupture. Ruptured ectopic pregnancy is a gynaecologic emergency, and can cause life threatening internal blood loss. Pain in your pelvic area is the most common symptom of ectopic pregnancy, but you may also experience nausea, vomiting, and dizziness. Some vaginal bleeding may occur.
How is an ectopic pregnancy diagnosed?
If you have missed a period and have any unusual pain or bleeding, you should contact your doctor. If your doctor suspects that you may have an ectopic pregnancy, he or she will likely conduct a pregnancy test, a pelvic exam, and request an ultrasound. This can help visualize the location of the ectopic pregnancy so treatment plans can be made.
How is an ectopic pregnancy treated?
An ectopic pregnancy needs to be removed, either using a medication that stops the growth of the fertilized egg, or through surgery. Surgery is usually done through a laparoscope – a small flexible tube with a camera and instruments that is inserted through a small incision in your abdominal wall. In emergency cases, you may need a larger incision.
Ovarian cysts
What is an ovarian cyst?
An ovarian cyst is a fluid-filled sac that develops on one of the ovaries each month. Usually these do not cause any pain, but sometimes they are associated with pelvic pain, especially during periods and intercourse.
What causes ovarian cysts?
Most ovarian cysts are related to normal ovulation. Several follicles develop on the ovary each month in preparation for ovulation. Sometimes one of these can keep growing and fill with fluid. Or the follicle that released an egg can seal back up and fill with fluid. It isn’t known why this happens. There are also other kinds of cysts that can develop that contain tissue (hair, skin, teeth), mucous, or endometrial tissue. Endometriosis can also cause ovarian cysts, called endometriomas. Rarely an ovarian cyst may be cancerous.
What are the symptoms of ovarian cysts?
Some cysts will cause no symptoms, and be found by chance. In some women, pain may be felt in the pelvic area or in the lower back and may worsen during menstruation. There may also be pain associated with bowel movements or intercourse. You may feel pressure in your pelvic area, and your breasts may be tender. It is rare, but cysts can rupture, causing severe pain, fever, and dizziness. Immediate medical attention may be required.
How are ovarian cysts diagnosed?
An ovarian cyst that is larger than 5 cm in width may be felt by your doctor during a pelvic exam and he or she may request an ultrasound for confirmation. Most cysts are less than 5 cm and can only be diagnosed on ultrasound and the majority of cysts less than 5 cm do not cause any symptoms.
How are ovarian cysts treated?
Many cysts disappear on their own within a few weeks or months. If the cyst is not going away or has worrisome features on ultrasound, or is causing you severe pain, you may have the cyst surgically removed. If you keep getting cysts, hormonal birth control methods can be used to stop ovulation and prevent the development of new cysts.

